Why Are Police Officers Overdosing From Fentanyl?
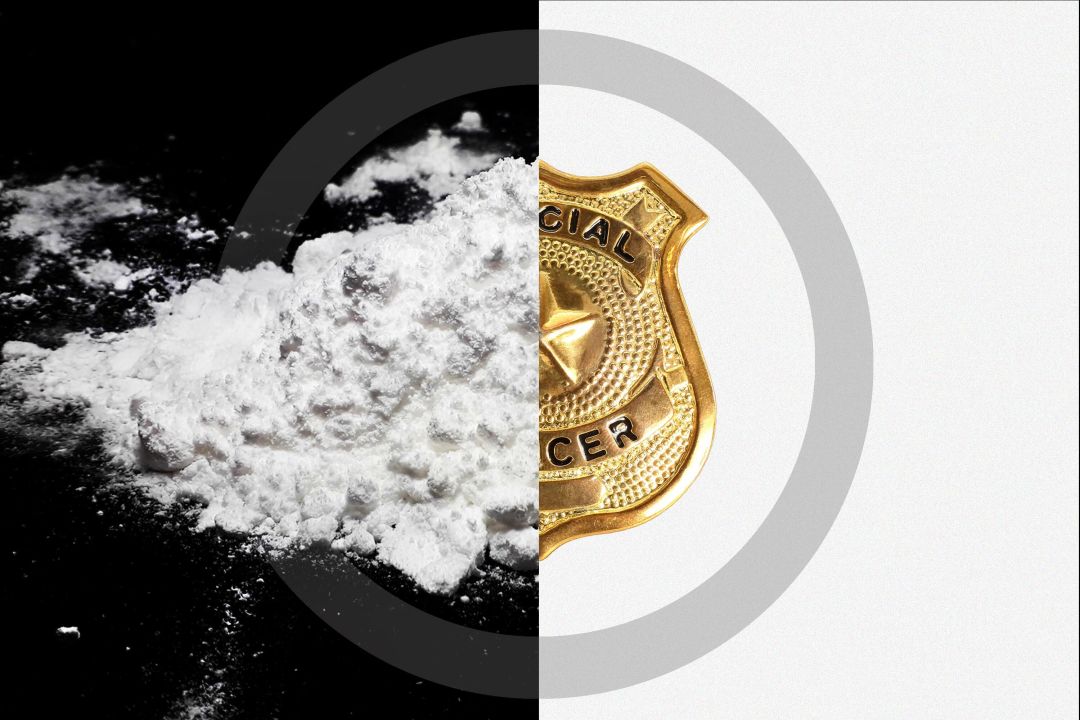
Image: Shutterstock Composite
Florida is no stranger to opioids. Between 2006 and 2012, the state was at the center of the opioid epidemic. During that time, Florida doctors made up 90 of the nation's top 100 opioid prescribers, and 85 percent of the country's oxycodone was prescribed in the Sunshine State.
Today, Florida has one of the highest fentanyl mortality rates in the country. Documents released by the governor’s office show that Florida saw more than 8,000 overdose deaths in 2021 and that, between 2015 and 2021, fentanyl-related deaths rose by 790 percent. Citing the fact that 75,000 Americans died from fentanyl overdoses in 2021, Florida Attorney General Ashley Moody wrote a letter to the Biden administration pleading with the federal government to classify fentanyl as a “weapon of mass destruction.”
In a December tweet, Moody also referenced a viral video of an Orlando-area police officer who allegedly overdosed after coming into contact with fentanyl. Footage caught on a body cam showed Tavares police officer Courtney Bannick calling for help from fellow officers during a traffic stop. She claimed a gust of wind blew a mysterious white powder into her nose and she began to feel strange. Assisting officers rushed to her rescue and administered three doses of naloxone (commercially known as Narcan) to prevent a fatal overdose.
This incident is part of a growing number of cases in which police have claimed to accidentally ingest potentially lethal amounts of the synthetic opioid. Medical experts, however, dispute these reports, claiming that it is not possible to overdose from faint contact with fentanyl. So how dangerous is contact with fentanyl? And why are police officers experiencing these symptoms?
Fentanyl is a fully synthetic opioid that is considered up to 50 times stronger than heroin. The Drug Enforcement Administration claims a lethal dose of fentanyl is just two milligrams, the equivalent of about 10 to 15 grains of table salt. The drug has been around since the 1950s and has many practical medical uses, like pain relief for cancer patients and epidurals for pregnant women, but the development of illicitly made fentanyl has increased exponentially over the last decade and infiltrated the black market drug trade.
Zach Siegel, a journalist who covers health, drugs and the criminal and legal system for magazines and his newsletter, says the proliferation of fentanyl is partly a consequence of market forces.
“Fentanyl is fully synthetic, unlike other opioids like OxyContin, which still require at least some part of the poppy plant,” Siegel says. “Opioids still need sunlight and land and poppy seeds in order to cultivate this crop to produce these drugs. What really changed the game with fentanyl, especially with the street and illicit markets, is that you don’t need farmers in Mexico anymore to grow poppies. You just need precursor chemicals you can acquire anywhere.”
Stories of accidental overdoses because of other drugs tainted with fentanyl are frequently in the news. Last March, five West Point cadets on spring break in Fort Lauderdale overdosed on cocaine contaminated with fentanyl. And this past Halloween, cable news shouted about fentanyl being in your child’s candy haul. Fear of a hidden scourge has gripped the nation.
Siegel says reporting on fentanyl is one of the most depressing and harrowing assignments he’s ever tackled. Still, he is skeptical of the stories of police officers overdosing. “It doesn’t look quite right when the cops are flailing about gasping for breath,” he says. “I looked at the body cam of [the Tavares] incident and at no point is the officer unconscious.”
Siegel says he’s seen many overdoses and there are a few telltale signs to look for. The first is that the person would be unconscious. If the person is white, their lips will be blue. If they are Black, the lips will be an ashen-gray. Overdoses of opioids cause death because they lead to respiratory failure, and the part of your brain that tells your heart to beat and your lungs to breathe shuts down. In that state, a person can only survive for a few short minutes.
“Not only is this officer gasping for breath and breathing, she is asking for naloxone,” Siegel says. “That defies the whole idea of an overdose. If people who were overdosing knew they were overdosing, they could hit themselves with naloxone. [Overdoses are] deadly because, when no one is around, no one is there to revive them."
Scott Huber, a lieutenant with the Sarasota County Sheriff’s Office, spent eight years as a narcotics detective. When he worked as an undercover officer, he would handle fentanyl, but never experienced adverse effects. “If you’re sitting in a car and buying from a dealer, you’re not going to do it with gloves and a mask on,” Huber says. According to Huber, there are no known cases of officers accidentally ingesting fentanyl in Sarasota County. Still, Huber helped create a policy at the Sarasota sheriff’s office that is intended to safely allow officers to handle and test for the presence of fentanyl while they are on duty investigating potential fentanyl cases.
“We had a policy for a long period of time that we were not going to be testing or field-testing our narcotics roadside without patrol deputies present,” Huber says. “For the last year, we have a policy in place and we are authorized and our deputies are authorized to field-test roadside any fentanyl or fentanyl-related product. We have a lot of protocols in place to ensure safety.”
One of those protocols is getting deputies “fit tested” every year. Each officer’s face is measured to make sure that their P100 respirator masks fit them airtight. If they fail the test, they are not allowed to handle fentanyl. Another protocol calls for having two deputies present and notifying dispatch. Also: Every deputy must carry naloxone. “The sheriff’s office here is progressive,” Huber says. “We were the first agency to have naloxone for their officers in the state.”
Florida does not afford such safety measures to its general population, however. Our state is one of a handful that has criminalized drug-test strips, which warn users of the presence of substances like fentanyl. The Florida Legislature has so far killed bills that would have decriminalized the lifesaving strips. Another bill to decriminalize the strips is set to make its way through this year's legislative process, but faces grim prospects.
Huber emphasizes the importance of officers being able to field-test for fentanyl.
“It’s really important for us to give the deputies the tools to do the job,” he says. "Imagine if ... we can’t make an arrest on side of the road because we can’t test the drugs. Two, three weeks go by, we get a report back from the lab and then get a warrant and make an arrest a month later. What happened in that month? ... How much fentanyl are you slinging on the street in the meantime?”
Huber says Sarasota has successful addiction diversion programs, like its jail recovery pod for addicts.
As for the officers around the country who claim to be overdosing on fentanyl, Huber is cautious about coming to a conclusion. He says that many of these cases are disputed and he doesn’t want to comment on the specific circumstances of the Tavares officer.
“We did a lot of research prior to implementing the policy and all of the research indicated that there has been zero lethal doses and it is very unlikely that someone would overdose in an outside environment with the amount of fentanyl or amount of incidental fentanyl that may or may not occur in those circumstances," he says. "It’s very rare.”
Huber continues, “A lot of the research indicates that there is a lot of fear and panic. Everybody reacts differently. You feel like you’re being exposed and your heart starts racing and you’re scared to death. Officers are legitimately afraid. They read the news and they watch stories. We wrote in our policy that officers don’t have to field-test if they don’t feel comfortable.”
Siegel believes officers experiencing overdose symptoms are actually experiencing something akin to a conversion disorder, a situation in which someone experiences physical symptoms without an underlying physiological cause.
“I think the best way to understand it is to think about what stress is," Siegel says. "Your mind is producing physiological symptoms. Your palms get sweaty and your heart starts racing. We’ve all experienced that.” To Siegel, these incidents often look like panic attacks. “They are gasping for breath, and when you are having a panic attack, that’s what you are doing. You’re trying to regulate yourself so you’re gasping for breath because it feels like you’re dying. And so I think that’s what’s happening.”
To listen to an extended interview with Siegel on the topic of fentanyl and overdoses, click here.



